As California prepares for another wildfire season, safety net health facilities are preparing to meet the needs of populations that will be affected in coming months. Given the continued effects of the COVID-19 pandemic and ongoing resource limitations, those efforts need to be focused where impacts are likely to be greatest.
CrisisReady is informing Direct Relief’s effort to assess how current wildfire risk, historical wildfire patterns, and historical use of shelters by affected populations overlap with the locations of safety net health centers in California. While predicting exact health care facility impacts and population movements for future disasters is not feasible, this analysis is able to provide information on patterns from past wildfire seasons that can inform current planning efforts.
The research team combined data from CalFire on wildfire risk zones (Fire Hazard Severity Zones) with information on historical emergency shelter utilization from the National Shelter System to provide assessments for 2059 safety net health centers in California. Of these, 23 are located in areas of Moderate fire risk, 9 are located in areas of High fire risk, 10 are located in areas of Very High fire risk by CalFire (Figure 1). While this approach provides information about direct risk to the facilities themselves, it likely underestimates risk to the populations they serve when facilities in low-risk zones are located near higher-risk areas.
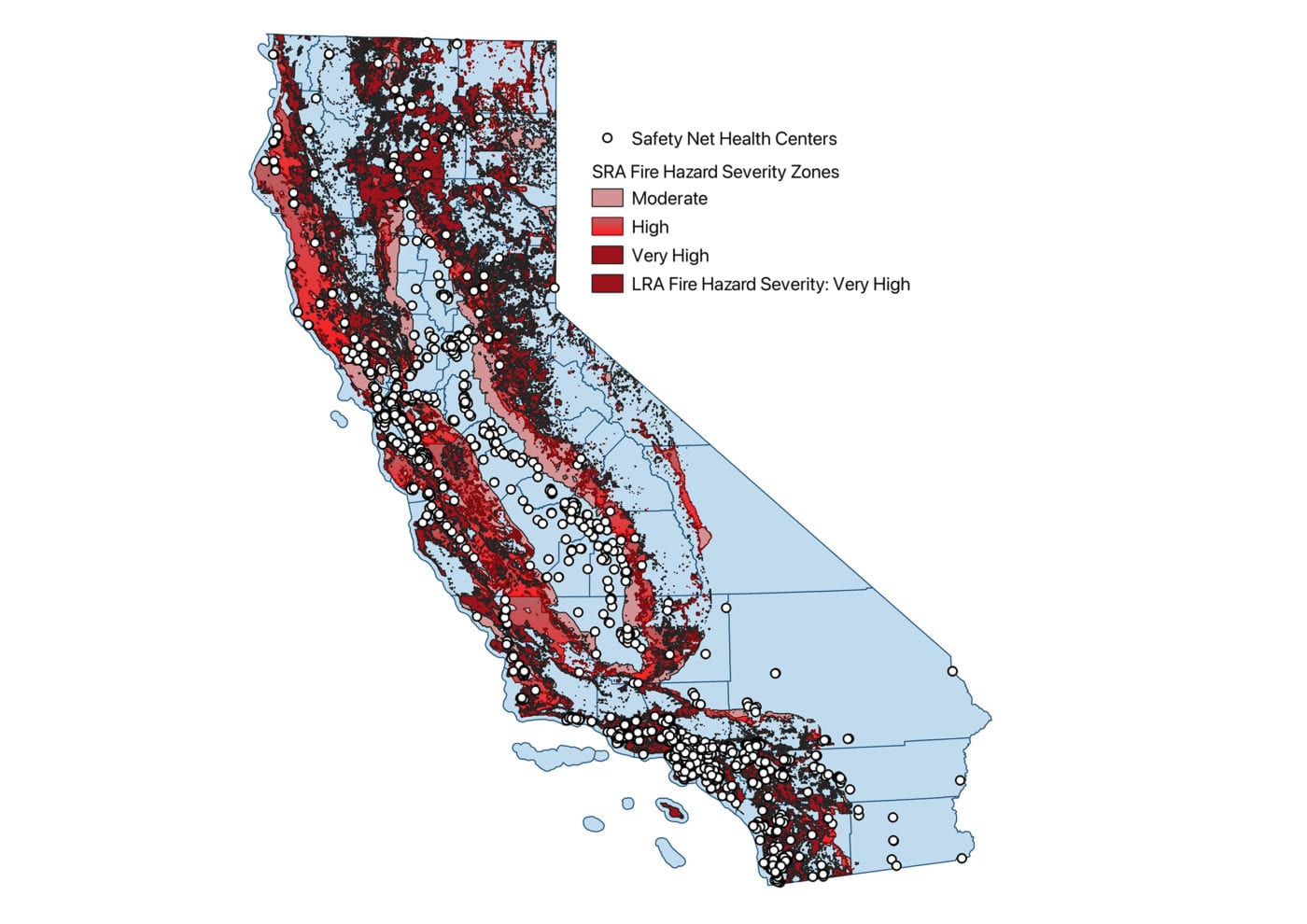
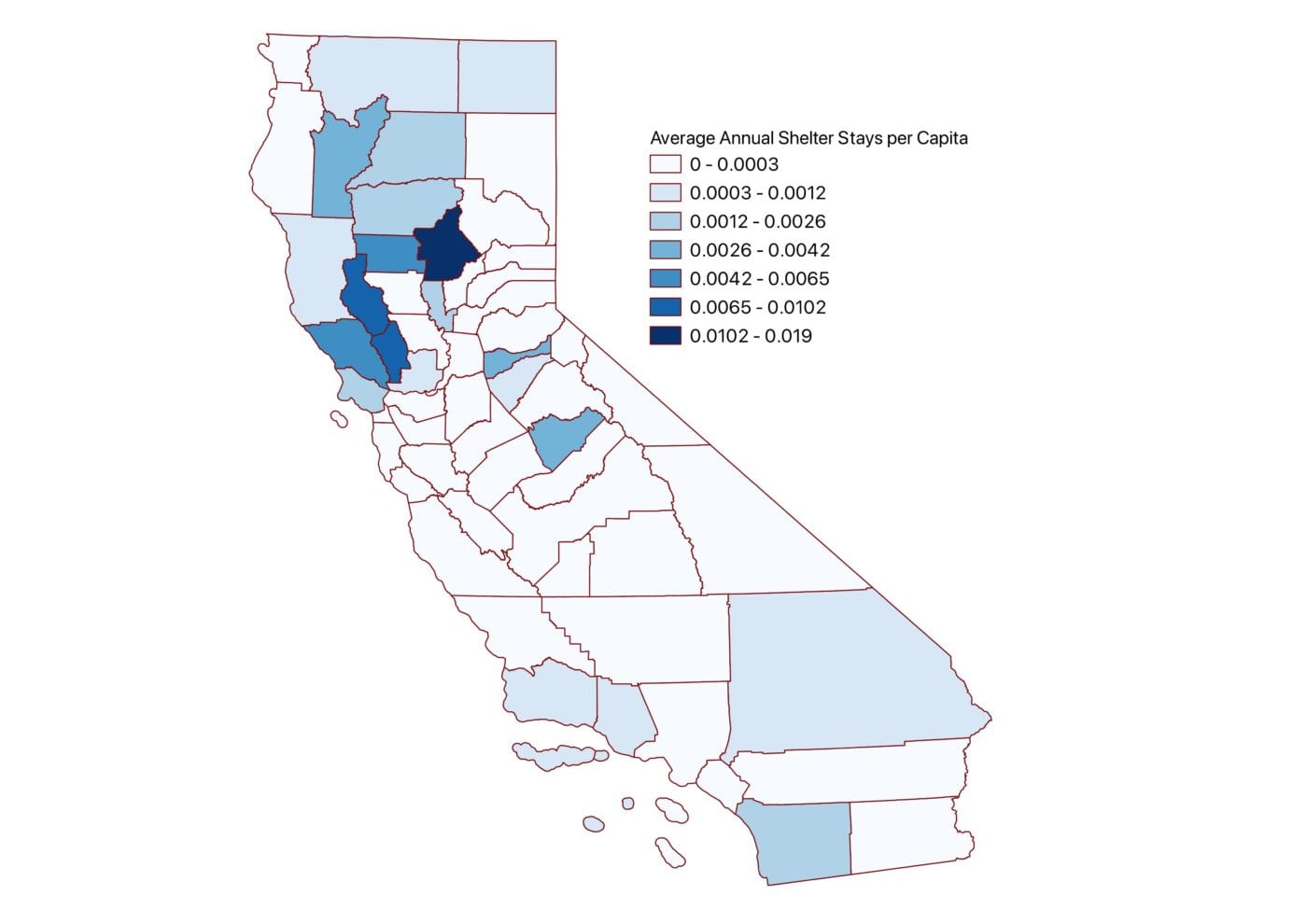
Historical emergency shelter utilization data can provide proxy information about population displacement during wildfires and the scale at which vulnerable persons need aid, including medical care, which they may access at nearby health centers. Spatial data on shelter use related to wildfires in California was obtained from the National Shelter System and was manually verified against media reports; sheltered population information for a small subset of fires was not available, and as a result, numbers presented here are very likely to be underestimated in some locations (Figure 2).
For the years 2007 to 2019, the total number of shelter stays, mean annual stays, and median annual stays were computed for a 25-mile radius around each of the 2059 safety net health centers. Use of shelters varied considerably by year, with a small number of major disasters such as the Camp Fire accounting for a substantial fraction of total shelter use. When data was examined on an annual basis, the team found that safety net health centers with high mean numbers of persons sheltering nearby often had been adjacent to a single devastating event that skewed the average upward. Information on median annual usage likely provides a more stable metric of expected local population displacement and relative population vulnerability in any given year, but both metrics have been provided given that exceptionally devastating events do represent the greatest demand on facilities, and should be considered in planning for future events. (Figure 3)
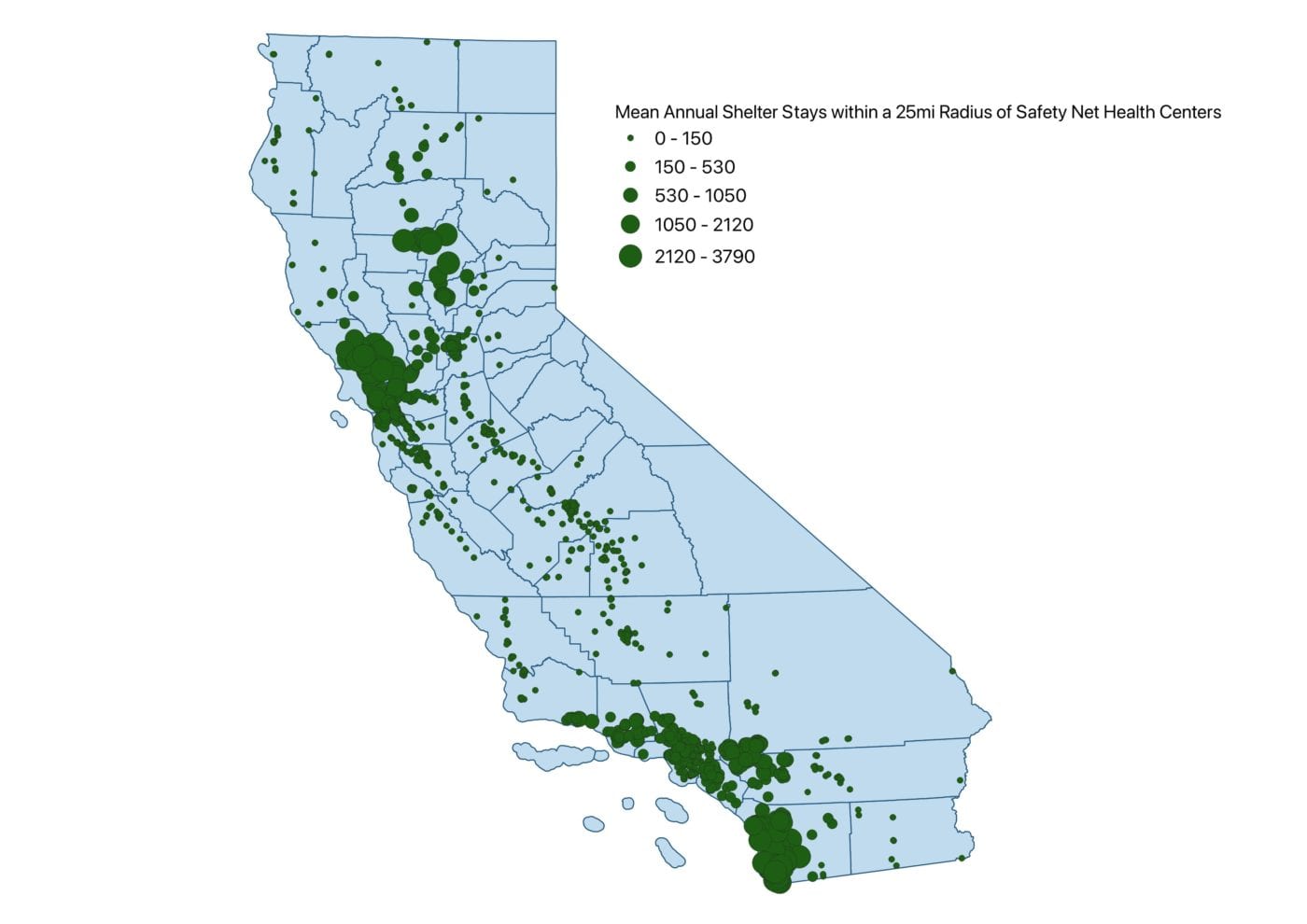
Within the limitations of these data sets, many safety net health care facilities in Los Angeles, San Diego, Butte, Glenn, Sonoma, Marin, and Napa counties have historically seen exceptionally large numbers of persons sheltering nearby, and should be particularly alert to needs for preparation to serve displaced populations during the upcoming fire season. In addition, facilities in rural parts of Northern California and inland Southern California may see high numbers of displaced persons relative to the baseline population, which also creates the potential to strain limited local resources.
Key steps should be taken now to prepare health facilities for what promises to be a difficult 2021 fire season. According to the National Interagency Fire Center’s National Significant Wildland Fire Potential Outlook, issued in May 2021, California is seeing warm, dry conditions and can expect above-normal fire risk in many areas. Similar dynamics contributed to a record-setting scale of wildfire activity in California in 2020. Long-term, the problem is getting worse, in part because of warmer, drier conditions related to climate change, as well as development and land use decisions.
As conditions become more challenging for safety net health centers and the populations they serve, resources need to go where they are most needed and facilities in high risk locations or serving high risk populations need to improve planning for future needs. Assessments of hazards and human impacts such as those presented here can help decision makers understand how to optimize resources and advocate for additional investment or support. Additional information on Direct Relief’s safety net preparedness efforts will be available at https://www.directrelief.org as fire season progresses.